A new landmark study reveals more First Nation’s families in Melbourne than ever before are benefiting from culturally-safe maternity care.
The service provides Aboriginal and Torres Strait Islander women care from a known and trusted midwife throughout pregnancy, birth and beyond.
Thanks to a multi-site research partnership called Baggarrook Yurrongi, which means Woman’s Journey, the Joan Kirner Women’s and Children’s Hospital at Sunshine Hospital was one of three Melbourne public hospitals to set up this new model of maternity care in 2017.
The Galinjera Maternity Program is a small team of dedicated midwives, obstetricians, social workers and a Koori Maternity Service Worker that supports First Nation families in Melbourne's West.
Galinjera means to come together and connect with love in the Wemba Wemba language.
Women and babies are offered care from a known (or ‘primary’) midwife throughout their pregnancy, labour, birth and in the immediate postnatal period. There are also several back-up midwives to support women and their families.
This continuity of care is associated with substantially better health outcomes, including reducing the risk of premature birth.
Midwives receive cultural safety training and are supported by workers from Western Health’s Aboriginal Health Unit, Wilim Berrbang.
Similar models of care were set up at the Royal Women’s Hospital and Mercy Hospital Heidelberg.
Results of new research led by La Trobe University in partnership with the Victorian Aboriginal Community Controlled Health Organisation (VACCHO) assessed the success of the new model of care at the hospitals from 2017-2020.
It found a remarkable uptake by Melburnian mothers during the study period. 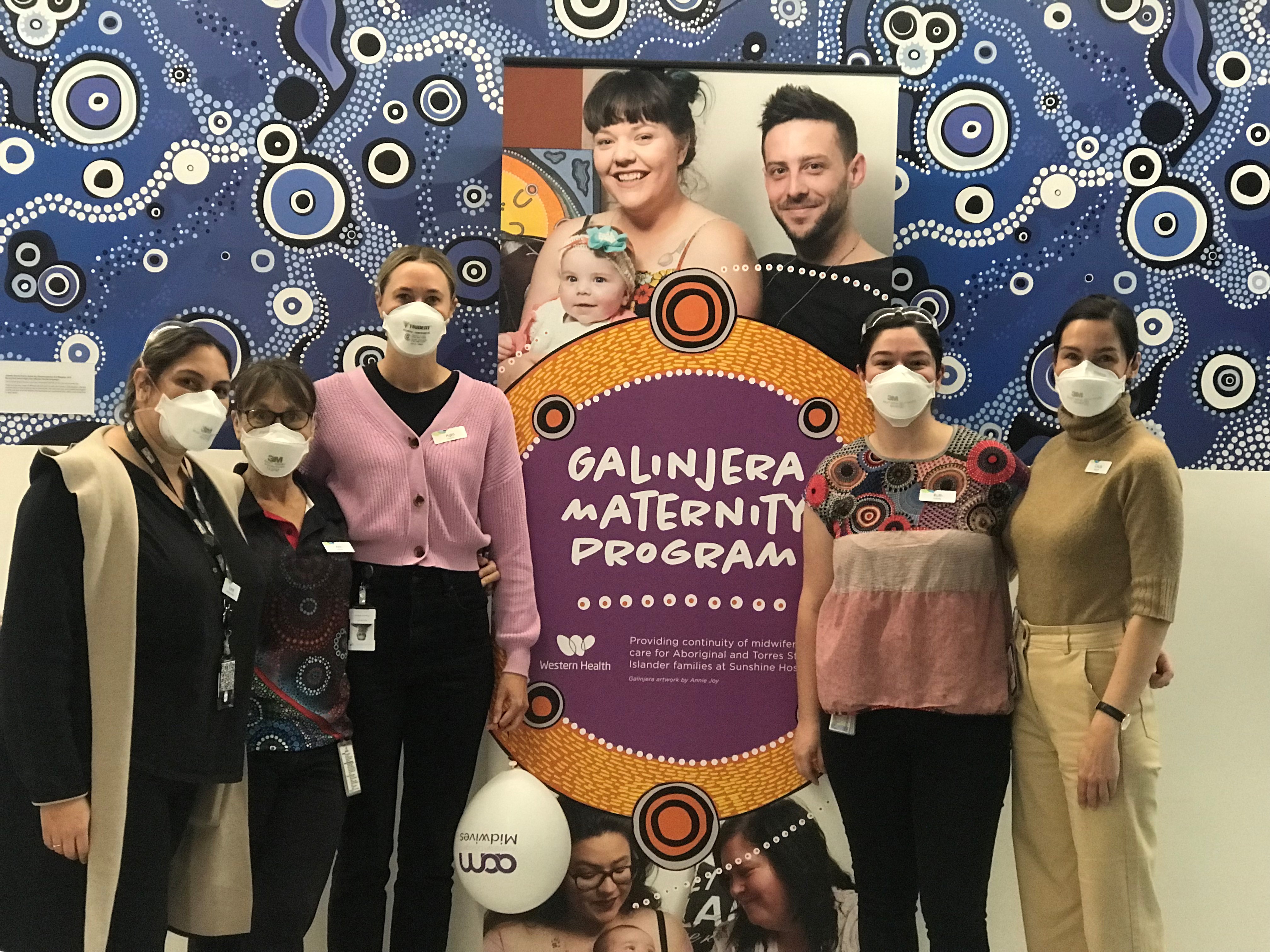
Under the partnership between the hospitals, researchers and First Nation’s health services, 703 of a total of 844 women having a First Nations baby received caseload midwifery care; an exponential increase.
Prior to this, over a similar timeframe, only 5.8 per cent of First Nations women (n=34) had ever received caseload midwifery at the three sites combined, compared with over 4,800 non-First Nations women.
Professor Della Forster, Professor of Midwifery at the Royal Women’s Hospital and La Trobe University, and co-lead of the study said:
“ We know that women who have midwife-led continuity are more likely to report being satisfied with their care, and to feel safe, informed, supported emotionally, and that their concerns are taken seriously.
“The enormous uptake of caseload midwifery by First Nations women in our study is likely to result in similar positive health outcomes for both mothers and babies.”
Women and babies in Melbourne’s West continue to benefit from this type of culturally-safe continuous care.
“We are delighted to have been part of this nation leading midwifery program, which provides best care to First Nation families in Melbourne’s West,” said Helen Sinnott, Director, Nursing & Midwifery at Joan Kirner Women’s and Children’s at Sunshine Hospital.
In The Lancet journal, eClinical Medicine, the authors said even more First Nation’s family could benefit from this collaborative and coordinated midwifery model if it was extended.
